Objective To review evidence-based knowledge of pediatric obstructive sleep apnea syndrome (OSAS).
Data Sources and Extraction We reviewed published articles regarding pediatric OSAS; extracted the clinical symptoms, syndromes, polysomnographic findings and variables, and treatment options, and reviewed the authors’ recommendations.
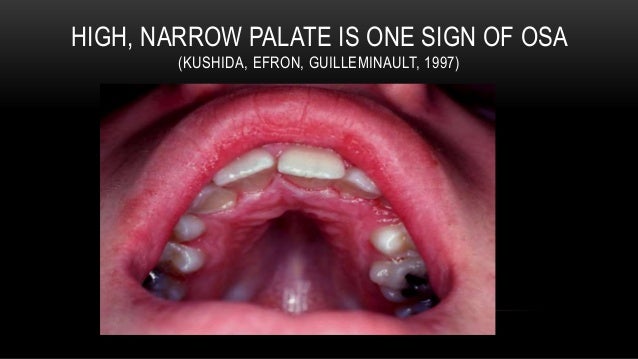
Data Synthesis Orthodontic and craniofacial abnormalities related to pediatric OSAS are commonly ignored, despite their impact on public health. One area of controversy involves the use of a respiratory disturbance index to define various abnormalities, but apneas and hypopneas are not the only abnormalities obtained on polysomnograms, which can be diagnostic for sleep-disordered breathing. Adenotonsillectomy is often considered the treatment of choice for pediatric OSAS. However, many clinicians may not discern which patient population is most appropriate for this type of intervention; the isolated finding of small tonsils is not sufficient to rule out the need for surgery. Nasal continuous positive airway pressure can be an effective treatment option, but it entails cooperation and training of the child and the family. A valid but often overlooked alternative, orthodontic treatment, may complement adenotonsillectomy.
Conclusions Many complaints and syndromes are associated with pediatric OSAS. This diagnosis should be considered in patients who report the presence of such symptoms and syndromes.
Understanding obstructive sleep apnea syndrome (OSAS) in children requires knowledge of the physiology of sleep and breathing. There is an immediate increase in upper airway resistance with sleep onset, with an initial “overshoot” in this resistance that decreases very quickly. Still, this resistance during established sleep is mildly higher than during wakefulness.
1There is also a slight decrease in tidal volume with sleep. This decrease will be more pronounced with the occurrence of rapid eye movement (REM) sleep. These mild decreases will be compensated by a slight increase in breathing frequency to keep minute ventilation normal. Breathing frequency decreases during the first 2 years of life but stays the same thereafter; it has been calculated to range from a maximum of 16 to 18 breaths/min in non-REM sleep and 17 to 19 breaths/min during REM sleep.
2,3
The obesity epidemic, evident in the United States and industrialized countries, has complicated the investigation of obstructive sleep apnea (OSA) and related syndromes. Fat distribution varies according to genetic, sex, and hormonal patterns and the inherent relationship among these 3 factors. It is common for fat to deposit in the abdominal region. Such abdominal obesity will lead to chest-bellows impairment, as seen in restrictive thoracic disorders. Although it may not lead to upper airway obstruction, abdominal obesity may worsen the poor gas exchange that may already exist because of OSAS. Sleep will always worsen the gas exchange in these subjects when they are in the supine position and when they achieve REM sleep. During REM sleep, the associated atonia eliminates contractions of the accessory respiratory muscles and the abdominal muscles, which engage in active expiration.
2,3 Also, REM sleep is associated with further flattening of the diaphragm’s position.
2 These physiological changes worsen gas exchange in subjects with abdominal obesity and may even lead to REM sleep–related hypoventilation with some degree of carbon dioxide (
CO2) retention. Upper airway impairment, per se, is not directly related to this
CO2 retention. It has, however, been hypothesized that abnormal gas exchange during sleep may impair the coordination of time-related contractions of both upper airway dilator muscles and inspiratory muscles.
Obstructive sleep apnea syndrome was described in children in 1976.
4 Although children may present with OSAS, the literature had established by 1982 that children had other abnormal respiratory effort patterns during sleep that were frequently associated with snoring and clinical symptoms.
5