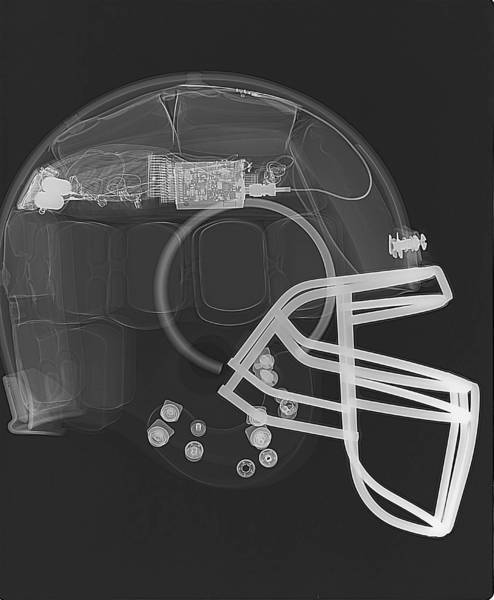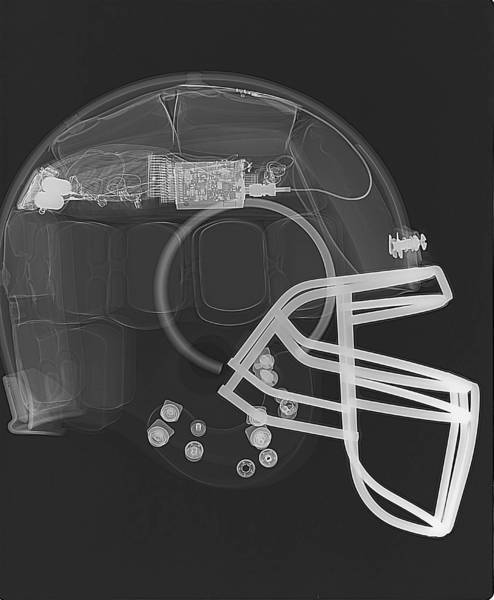
For almost a decade, helmet-maker Riddell has gauged the frequency and severity of head impacts through helmets lined with sensors that communicate wirelessly to the sidelines. But Able "wanted to develop a technology that provided impact data for all sports, not just helmeted sports."
The result is the X2 Impact, an electronics-packed mouth guard that records direction, force and number of impacts to the head, then wirelessly sends the information to sideline staff. Able worked with engineer Christoph Mack and Seattle-based Anvil Studios to develop the "boil-and-bite" mouth guard, which has a gyroscope, accelerometer, radio and chipset inside to record and relay information.
Together with research partner Stanford University, whose football and women's soccer and field hockey teams are wearing the mouth guard, X2 is collecting data that it hopes will help coaches and medical professionals better determine when a concussion may have been suffered or at least when to pull an athlete off the field.
Neither monitoring system tells a trainer if a concussion has been suffered — unlike other injuries, a concussion isn't necessarily easy to see and instead is determined by symptoms that may (or may not) include nausea, dizziness, confusion, clumsiness and forgetfulness. Also, Able said, "so many times kids will hide their head injuries because they don't want to sit on the bench."
"We're an information and awareness tool," said Able, about X2. "We're giving information that helps a trained medical professional make a better assessment of a kid."
Some college trainers are immediately notified via pager with Riddell's system if an athlete has suffered an abnormally hard hit, so they can focus on that player.
Studies have shown that long-term exposure to concussion and blows to the head can result in Chronic Traumatic Encephalopathy, which can cause memory loss, confusion, impaired judgment, impulse-control problems, aggression, depression and eventually, progressive dementia, according to Boston University's Center for the Study of Traumatic Encephalopathy.
Game-changer
The mouth guard joins the nearly decade-old Head Impact Telemetry System and Sideline Response System, owned and co-developed by Riddell and product development firm Simbex. Data on 1.8 million on-field head impacts have been collected through the HITS system, leading to dozens of published studies and several rule changes, including:
Brown and Dartmouth successfully lobbied the Ivy League to eliminate in-season, full-contact practices and reduce them in preseason because of how many head impacts athletes were exposed to. "Reducing impact exposure will ultimately reduce athletes' risk of concussion," explained Thad Ide, Riddell's senior vice president of research and product development.
A study involving HITS data on 7- and 8-year-olds prompted several rule changes in Pop Warner Football this June: No full speed, head-on (face-to-face) blocking or tackling drills are allowed when players are more than 3 yards apart and, full contact will be reduced to a maximum of one-third of practice time. The study was conducted by Virginia Tech-Wake Forest University researchers.
The NFL moved the kickoff line up 5 yards to lower the number of collisions during kickoff returns, in part based on HITS data.
Virginia Tech uses the HITS system to rank football helmets by their concussion-reduction capabilities.
"Virginia Tech, UNC, Brown and Dartmouth, Indiana and Purdue — all of them use the (Riddell) system and study and pool their data," Ide said. "They're just scratching the surface of what they can learn from that data."
Coaches have used the system to change drills or plays that increase head-impact exposure. "If you have someone review the data regularly," added Ide, "you can look at the number and types of hits of a particular player and compare that to other players in that same position and skill level to determine if they're using their head improperly or too much.
"There's so much that's not known about concussion and impact exposure, so the research part is extremely important right now in order for us to make better choices in the long run."
For information on concussion and youth sports: cdc.gov/concussion/pdf/coaches_Engl.pdf
For how to recognize possible signs of concussion, go to cdc.gov/concussion/sports/recognize.html
 Sleep Med. 2012 Jun;13(6):621-31. Epub 2012 Apr 13.Psychological Sciences, The University of Melbourne, Melbourne, Australia.
Sleep Med. 2012 Jun;13(6):621-31. Epub 2012 Apr 13.Psychological Sciences, The University of Melbourne, Melbourne, Australia.